Platelet-rich Plasma (PRP) Prolotherapy
Many people have heard the term “platelet-rich plasma” in news stories in connection with athletic injuries or facial treatments, however do not realize that when platelet-rich plasma is injected into and around a joint, it is actually a type of Prolotherapy. In fact, platelet-rich plasma has been used as a formula in Prolotherapy since around 2005. Platelet-Rich Plasma (PRP) Prolotherapy has been shown to be effective not only for older injuries but also for recent ones,[1] making it ideal for athletic injuries. It has also successfully been used in the treatment of osteoarthritis (OA) and helpful for cartilage repair.[2]
The History of Platelet-rich Plasma
For many years, it had been observed that using platelet-rich plasma during a surgical procedure could improve how well a patient healed after surgery.[28] Orthopedic surgeons had been using PRP as early as the 1970s to assist in the healing of fractures and bone grafts with good results. However, preparing platelet-rich plasma required a large quantity of a patient’s blood as well as big, expensive equipment; thus, the use of platelet-rich plasma was limited to hospitals.[29] By the 1990s, platelet-rich plasma machines were getting smaller and more portable. Multiple reports emerged showing dramatically improved healing when platelet-rich plasma was used during maxillofacial dentistry, periodontal surgery,[30] cosmetic surgery,[31] and skin grafting.[32]
These successes encouraged the use of platelet-rich plasma in sports medicine for connective tissue repair. In 2006, Mishra and Pavelko, associated with Stanford University, published the results of a study that used platelet-rich plasma injections for chronic tendon problems.[33] This study reported a 93 percent reduction in pain at two-year follow-up. Then, in 2008, just before the Super Bowl, Pittsburgh Steelers wide receiver Hines Ward received platelet-rich plasma injections for a knee injury. The Steelers went on to win Super Bowl XLIII, and Ward credited platelet-rich plasma with allowing him to get back in the game. Ward’s success with platelet-rich plasma was publicized on national television,[34] making platelet-rich plasma more widely known. In 2010, the Mayo Clinic Health Letter discussed the use of platelet-rich plasma for enhanced healing of injured tendons.[35] Since then, not only has the use of platelet-rich plasma spread to the general public, but it has expanded to traditional orthopedic and sports medicine circles and continues to be used by many high-profile athletes.[36]
Platelet-rich Plasma Basics
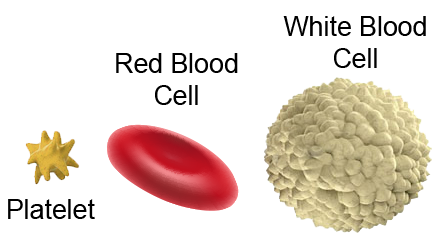
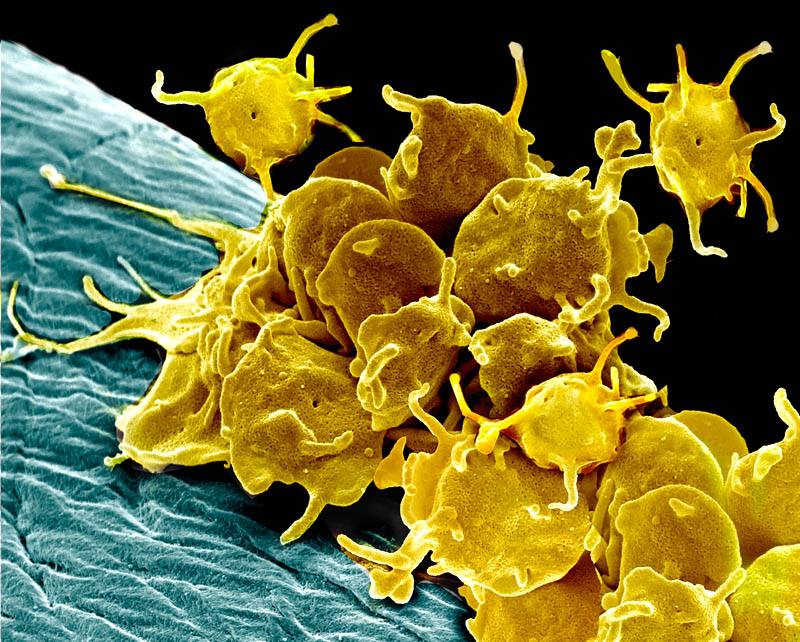
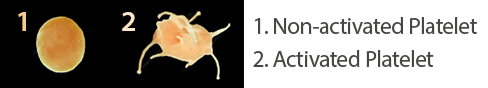
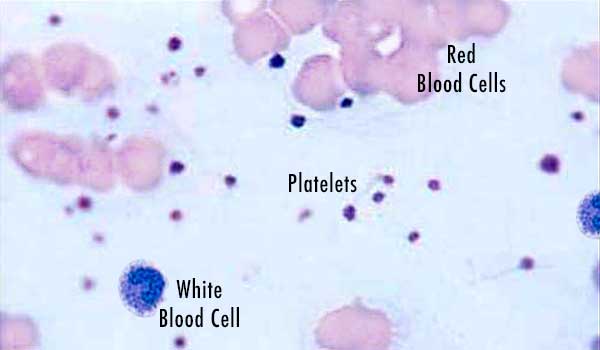
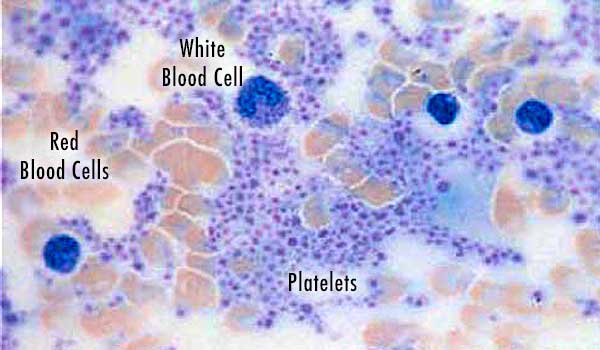
Our blood is composed of these basic elements: red cells, white cells, and platelets, all suspended within a liquid called plasma. Platelets are small, plate-shaped bodies (hence the term “platelets”) which contain growth factors and other proteins that control natural wound healing.[3] Blood can be withdrawn from an individual, then placed in a machine that spins it (a “centrifuge”), and these blood components will separate from each other.
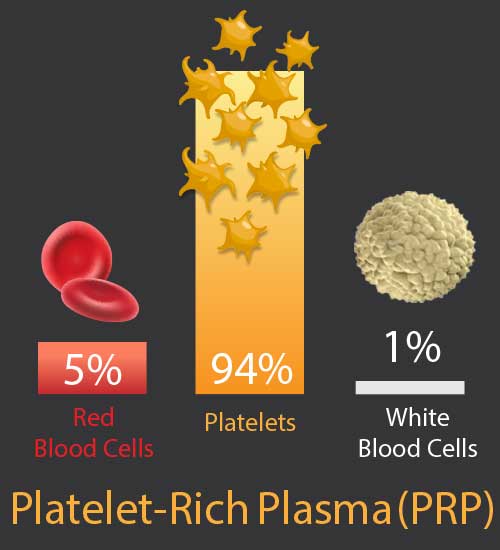
The definition of PRP, as used in musculoskeletal medicine, is autologous blood (autologous: taken from the same person it is returned to, from the Greek auto for “self”) in which platelets have been concentrated above their normal (baseline) levels.[4] By concentrating the blood in this way, the growth-factor rich platelet portion of the blood goes from 6 percent to 94 percent, increasing potential healing ability dramatically.
The PRP Procedure
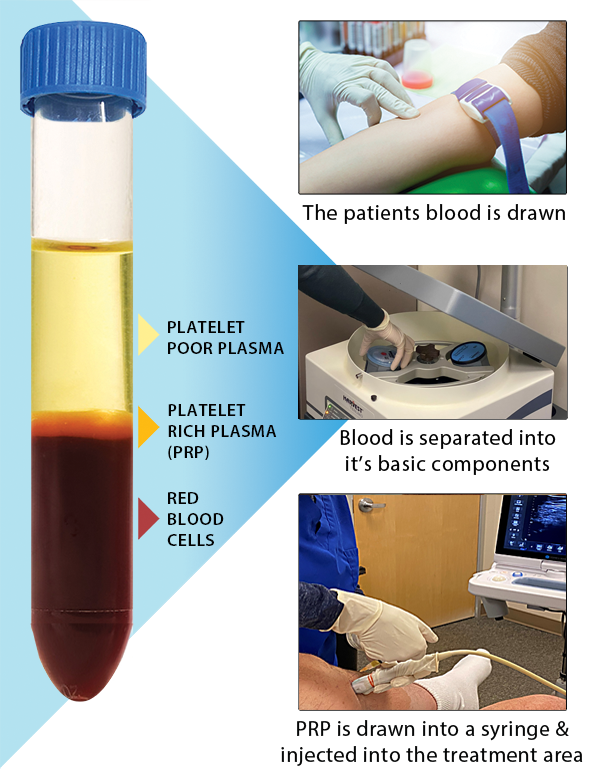
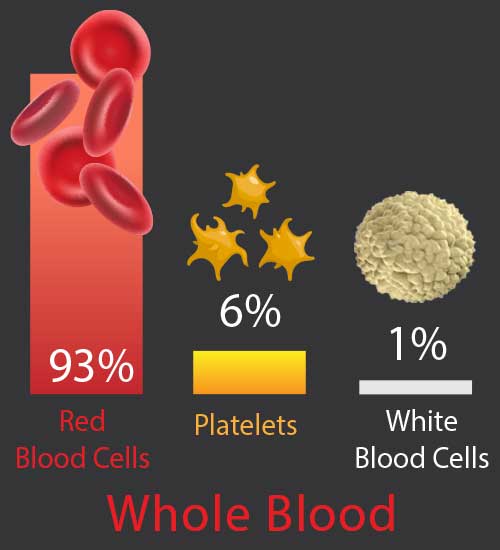
Platelets 6%, White Blood Cells 1%.
Platelet-rich Plasma in
Musculoskeletal Medicine
As of March 2022, over 14,113 medical studies regarding platelet-rich plasma appear in the US National Library of Medicine’s PubMed database,[5] and the term “platelet-rich plasma” appears in 1,510,000 references in Google Scholar,[6] with more being added every day. Platelet-rich plasma has been found to be effective for use in ligament and tendon injuries,[7] chronic tendinopathies,[8], osteoarthritis,[9] knee meniscal tears,[10] cartilage repair,[11] elbow pain[12] and other sports injuries,[13] patellar tendinopathy and muscle strain,[14] muscle tears,[15] jumper’s knee,[16] Achilles tendinopathy,[17] plantar fasciitis,[18] temporomandibular joint (TMJ) disorders,[19] disc disease including cervical and lumbar disc herniations,[20] sacroiliac joint dysfunction,[21] hip pain[22]and other spine and low back pain[23] (even in older patients[24]), biceps and rotator cuff tears and tendinopathy,[25] and other musculoskeletal and orthopedic injuries.[26] Although discussion and some controversy exist in regards to which is the best concentration or type of PRP to use for various conditions,[27] there seems to be general agreement that platelet-rich plasma enhances musculoskeletal healing.
How Platelet-rich Plasma
Enhances Healing
When platelets are injected at the site of an injury and then activated (turned “on”, discussed later in this chapter), they release growth factors that signal for local adult stem cells (repair cells) to come to that injury site, which increases the rate of healing[28] ,This makes sense because the initial number of platelets at a wound site is directly related to how well and fast an injury heals.[29] And growth factors released by PRP have been shown to help increase blood supply and new blood vessel formation, a process called “angiogenesis” (angio for “blood vessel”; genesis for “new”),[30] important in tissue repair.[31]
Not All Platelet-rich Plasma Is Equal
As the use of platelet-rich plasma has grown, so has the demand for, and availability of, platelet-rich plasma–concentrating machines and methods; several manufacturers now make these systems. There are also doctors who “do it themselves” using a regular type of centrifuge rather than one of the systems developed for this purpose. The basic difference among all these various methods is 1) the amount of concentration of platelets (how many times a person’s normal levels (called “baseline” levels) and 2) the presence and number of red or white blood cells.[32]
Platelet-rich Plasma Concentrations Affect Stem Cell Populations
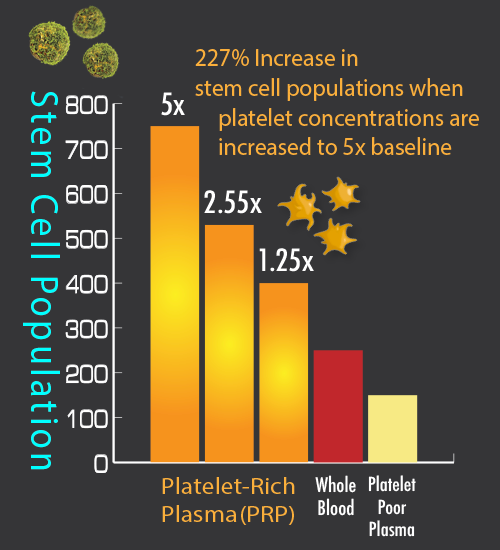
There is debate in the medical community about what is the best platelet concentration or cell types for different conditions; however, most data supports a platelet concentration of four to six times a patient’s normal level (baseline) for most musculoskeletal problems.[42] More specifically, since the average normal patient’s platelet count is 250,0000 platelets per microliter, this means that the magic number is 1.0 million to 1.5 million platelets per microliter (4 to 6 times normal baseline). This concentration has shown better tissue regeneration when compared to lower platelet concentrations. It also seems that much higher concentrations could have an inhibitory effect,[43] which may decrease effectiveness[44].
Therefore, four to six times baseline has become the most commonly used concentration for platelet-rich plasma and this concentration range is known as “high-density.”
Remember that platelets work by sending out biochemical messages so that nearby available stem cells will come and help repair injured areas. It has been found that when high-density PRP is used there is a stronger stem cell response when compared to whole blood or PRP with lower platelet concentrations (see figure: Stem cell response related to platelet-rich plasma concentration).
Red and White Blood Cells
The other difference between PRP is the number of red and white cells. Keep in mind that most of the red cells are already removed in the making of platelet-rich plasma: whole blood is 94 percent red cells as compared to only 5 percent red cells in PRP (see figure: Cell ratios in whole blood and PRP diagram above). However, even though the remaining red cells are greatly diminished, it is believed that any red cells may still cause unnecessary aggravation after treatment. One issue has been that removing too many red cells may greatly reduce platelet levels since some platelets are within the red cell layer. Fortunately, recent developments in technology now permit the ability to remove most of the red cells while still maintaining high platelet counts. Another issue is that with Prolotherapy, we may prefer this additional red blood cell irritation to “wake up” certain tissue types that are not healing. Therefore, both formulas are used in Prolotherapy—the low red cell (“yellow”) and the regular red cell (“red”) —depending on the area treated, intended result, physician and/or patient choice and treatment plan.
Regarding white blood cells, some physicians argue that white cells may cause too much pain and should be reduced, especially in joints.[45] However, typically, white cells constitute only 1 percent of both whole blood and platelet-rich plasma, and therefore a very small percentage of the treatment formula (see figures: Cell ratios in whole blood and PRP diagrams above). Also, white cells are very difficult to remove without seriously sacrificing platelet numbers. [46] Most physicians also agree that white cells are important and improve wound healing; furthermore, white cells have antibacterial properties that are thought to potentially help reduce infection risk from, or after, the procedure (as long as also done under appropriate sterile conditions of course.)[47] Therefore, it is generally agreed in the medical community that white cells are desirable and should remain in platelet-rich plasma formulas.[48]
How Platelet-rich Plasma is activated
In order to release growth factors, platelets must be activated. The activation process occurs in different ways. In a hospital setting, the surgeon activates platelet-rich plasma by mixing it with a commercially available protein called “thrombin.” Thrombin thickens the PRP and causes a fast release of growth factors; this combination is then put on the desired tissue during surgery to help with healing. When PRP Prolotherapy is done in an office setting, some physicians add a very small amount of calcium chloride to the local anesthetic or to the platelet-rich plasma just prior to injection, which stimulates a slow release of platelet growth factors.[49] However, as it turns out, thrombin protein is also a natural component of connective tissue. That means that thrombin will naturally be released when the injection needle tip pierces the connective tissue that is being injected.[50] This is why Prolotherapy technique, which involves some needle peppering of the injection site, is important, especially if no other activating method is done. This needle irritation not only releases natural thrombin but also, as discussed earlier, “wakes up” nonhealing tissue so that platelets are directed where to start repair.
Cortisone versus Platelet-rich Plasma
Cortisone injections are commonly recommended for the treatment of joint pain. However, the use of cortisone is controversial because it tends to break down, rather than repair, joints and connective tissue, especially if done repeatedly. Current evidence now supports platelet-rich plasma to be more effective than cortisone for treatment of joint and connective tissue issues,[51] especially long term. A well-designed,two-year, randomized, controlled, blind trial (meaning patients did not know which formula they were receiving), with a significant test group of 100 patients investigated cortisone versus platelet-rich plasma injections for elbow tendon problems. The researchers concluded that platelet-rich plasma reduced pain and increased function significantly, exceeding the effect of corticosteroid injection even after two years.[52] A similar study in 2017 agreed.[53] These two treatments were also compared for use in chronic, severe plantar fasciitis and concluded: “PRP was more effective and longer lasting than cortisone injection.”[54] Platelet-rich plasma has also been found to be a “superior treatment option” versus cortisone for lumbar facet (low back joint) injections, with longer lasting effectiveness.[55]
Platelet-rich Plasma for osteoarthritis and cartilage pathology
Multiple studies continue to emerge confirming the effectiveness of platelet-rich plasma for osteoarthritis (OA), Platelet-rich plasma also appears to have a protective effect on cartilage.[56] For more details see this article: Clinical update: Why PRP should be your first choice for injection therapy in treating osteoarthritis of the knee (2018)
Platelet-rich Plasma safety concerns/risks
Like Dextrose Prolotherapy, PRP Prolotherapy is low-risk and has few side effects. Concerns have been raised that the use of platelet growth factors can result in unwanted overgrowth of tissue; however, there have been no documented cases of hyperplasia (overgrowth), carcinogenesis (cancer), or tumor growth associated with the use of platelet-rich plasma that is autologous (taken from the same person it is given to).[57} Platelet-rich plasma growth factors do not enter the cells they are interacting with; rather, they act by binding to the outside of these cells.[58] This interaction causes normal healing but at a faster rate. Therefore, it has been concluded that platelet-rich plasma has no ability to induce tumor formation.[59] In addition, because the blood used in PRP Prolotherapy is taken from the same person it is given to, the risks of allergy or infectious disease are considered negligible.[60] As mentioned earlier, evidence also exists that platelet-rich plasma may have an anti-bacterial effect,[61] which also improves safety of the treatment when done under appropriate sterile conditions.
PRP Prolotherapy versus Dextrose Prolotherapy
Both PRP and Dextrose Prolotherapy have been shown to stimulate natural healing.[62] Both can be effective, and both should be considered in the treatment plan for connective tissue repair. PRP Prolotherapy, however, may be deemed more appropriate in cases where the tissue or joint has become degenerated, there is osteoarthritis present or the problem is older and more chronic. When platelet-rich plasma is the formula used in Prolotherapy, it provides not only needed irritation (concentrated platelets are aggravating!) but also growth factors that provide a jump-start on healing. Using platelet-rich plasma is like adding fertilizer to newly planted seeds versus just planting the seeds; the condition of the “soil” can help to determine which formula is the best choice. Platelet-rich plasma may also be preferred over dextrose in cases of a tendon sheath or muscle injury; these areas are occasionally, but not typically, treated with dextrose.
Other factors to consider are that platelet-rich plasma is a more aggressive formula than dextrose; therefore, it can be more aggravating and uncomfortable for the patient afterward. The cost of PRP Prolotherapy is also higher than for Dextrose Prolotherapy because of the additional materials needed. Another difference is that PRP Prolotherapy seems to stimulate multiple healing episodes, sometimes creating more “ups and downs” in pain levels during the weeks following a treatment. With dextrose, on the other hand, there is usually only an initial period of discomfort, although there are variations from patient to patient. As a general rule, fewer treatments are needed with PRP than with dextrose. The bottom line is there are several factors to consider, and the determination of which type of Prolotherapy to use is made on an individual basis after careful evaluation and discussion between the doctor and the patient of all factors, including patient preference.
Case Report: Dentist

I continued to have pain shooting up and down my hand every time I turned the knob to open a door, twisted the lid off a jar, or basically otherwise tried to use it. I was concerned that if I didn’t receive proper treatment, it could eventually shorten my career. I decided that wasn’t an option.
I had heard about platelet-rich plasma (PRP) and regenerative medicine at a dental implant residency program; however, it wasn’t until I heard about it again later from a medical colleague that I began to look into this emerging yet promising treatment option. Having a basic medical understanding about this particular type of treatment, I wanted to find someone who was skilled and specialized to perform it.
While I was researching PRP and Prolotherapy physicians, Dr. Donna Alderman’s name kept coming up again and again, and I am glad it did. After the initial consult, she was optimistic that she could help me with PRP, sparing me from other therapies (and possible overtreatment). She was right! After only two PRP sessions, my wrist is now 99 percent better. I am able to work out again and do my normal daily activities, tending to my busy dental practice and all my patients while being virtually pain free. I definitely recommend PRP Prolotherapy to anyone who wants to handle their pain effectively without the burden, expense, and uncertainty of surgery. Yes, it is that good!
Ray Cros, D.M.D.
Family and Cosmetic Dentist