Common Causes of Musculoskeletal Pain,
How Prolotherapy Regenerative Medicine Helps
Connective tissue weakness is the most common cause of long-lasting musculoskeletal pain.

Injuries involving ligaments and tendons (connective tissue) are slow to heal because the blood supply there is poor (see Prolotherapy Basics). After an injury, healing is strongest for the first few weeks and continues for about six weeks. However after this period of time this ability to heal is reduced or gone. The result of incomplete healing is weakness of that tissue, known as connective tissue weakness (also called “laxity), which, if it continues, results in instability of that joint and eventually chronic musculoskeletal pain. In fact, connective tissue weakness is the most common cause of long-lasting musculoskeletal pain, and is exactly what Prolotherapy addresses.
What causes Connective Tissue Weakness?
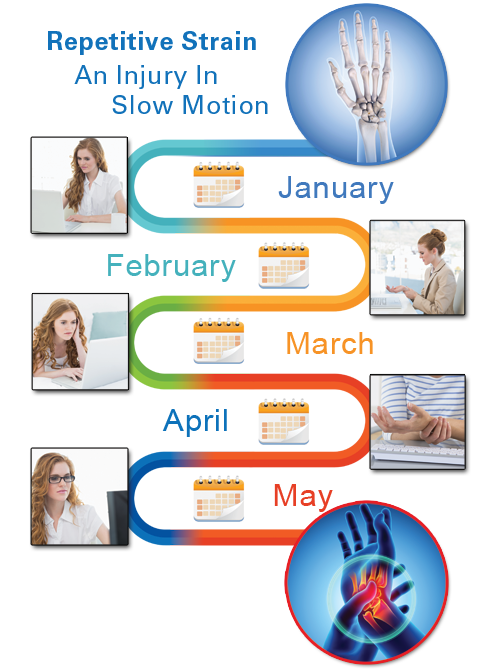
Connective tissue weakness can result from an obvious accident or injury, such as a motor vehicle accident or sports injury. However, it can also, commonly, result from smaller, repetitive traumas that are not as obvious. A few examples of repetitive motions, which if done routinely may result in injury, are a mechanic turning a wrench, a delivery worker lifting boxes, a person texting on his/her cell phone, or an administrator or student typing at a computer. Many active individuals can experience these types of small ligament or tendon injuries without ever knowing what specifically caused them, resulting eventually in connective tissue weakness and pain.
Joint and connective tissue injuries are also common in athletes. Ideally, a player with a known ligament or tendon injury is put on the “injured list” and not allowed to play until it is believed that he/she is fully healed. However, as discussed earlier, even if someone is feeling better, because of the poor blood supply the tendency is that most of these types of injuries do not result in 100 percent healing[1], leaving the area a little weaker and the player more susceptible to re-injury. Additionally, someone may not even notice small injuries and so continue to use the weakened area because it has not yet gotten on his/her “radar.” Indeed, small, repetitive injuries can accumulate in any joint until one day there is unrelenting pain.
The Challenge of Connective Tissue Healing and Collagen Repair
An important element of connective tissue healing is the rebuilding of collagen—a strong protein that is a major component of ligament and tendon tissue. The word collagen comes from the Greek kola for “glue,” and gennan for “to produce.”[2] This strong, glue-like protein is critical to healing an injured ligament or tendon. Various lifestyle factors can reduce or prevent collagen repair, such as poor nutrition, poor-quality sleep, smoking, and certain medications.
Certain nutrients and micro-nutrients are needed for proper collagen repair. For example, without vitamin C, the body cannot properly repair and rebuild collagen. Scurvy, a disease common among sailors in the eighteenth century, is an extreme example of vitamin C deficiency that prevents normal collagen repair, resulting in poor wound healing and joint pain, among other symptoms. The problem of scurvy was solved when a daily lemon, lime, or orange was added to the sailors’ previously citrus-free diet. While this is a dramatic example of a severe nutritional deficiency, more subtle deficiencies may also exist in an individual that influence how his/her body repairs and makes collagen (for more information see The Nutrition Connection).
Another factor affecting collagen repair is sleep. Sleep is important for repair and regeneration of normal, day-to-day small connective tissue injuries and joint wear and tear.
This is because when we have quality sleep, our body makes growth hormone, important for collagen and other tissue repair. A good night’s sleep will generally repair these small, daily injuries. However, if sleep is disturbed or not adequate, even tiny injuries can accumulate, resulting in pain.[3]
Cigarette smoking also diminishes the body’s ability to build and repair collagen. This is why smokers get facial wrinkles at a younger age than nonsmokers—collagen in the skin is not being adequately repaired—and also why smoking is not recommended before or right after surgical procedures when healing is important.[4] Ingredients in cigarettes, such as nicotine and other chemicals, prevent adequate collagen repair.[5] Even if the person quits smoking later, if he/she was smoking when the body was supposed to be healing, the damage has already been done.
Another possible reason for incomplete connective tissue healing is the use of anti-inflammatory medications,[6] or other immune system lowering pain medications, at the time of the injury. Since inflammation is a necessary component of connective tissue healing, the use of anti-inflammatory medication for these types of injuries has been seriously questioned[7].
Incomplete Connective Tissue Healing Leads to Joint Instability
For the aforementioned reasons, joint connective tissue may not heal sufficiently after an injury, leaving the ligaments and tendons around the joint weaker. As you can imagine, this will logically result in the joint having less support around it, and will become less stable. If this instability does not resolve in a reasonable period of time, the body perceives this as a problem it needs to solve. Even a small amount of excess motion in a joint can trigger the body to try to resolve this problem.
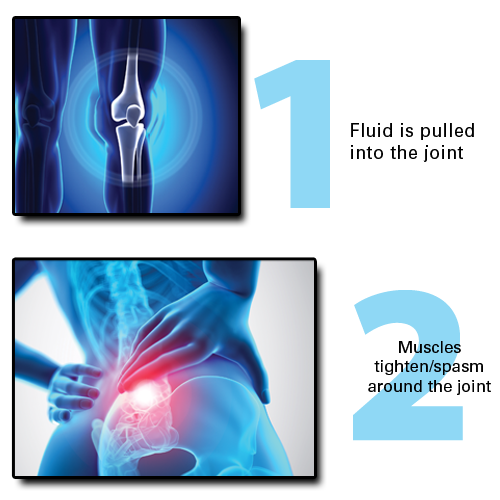
The body responds to joint instability in three main ways. The first is that fluid is pulled into the joint or joint area. This frequently occurs in areas such as the knees, where cysts (fluid-filled sacks) or effusions (fluid in a joint) can occur in the body’s attempt to stabilize the joint.
Second, the muscles over the area will tighten, creating muscle spasm. This occurs especially where there are large muscle groups such as the back. And if muscle spasm continues for too long, the muscles may develop “trigger points”—areas of perpetual tightening. These trigger points can be felt as muscle knots, which are sore and tender to the touch and can “trigger” pain. Thus the body’s attempt to fix the initial problem (instability) can result in other problems: chronic joint swelling and/or muscular tightness and spasm!
Joint Instability Leads to Pain and, Ultimately, Osteoarthritis
If instability in a joint continues, the body initiates a third effort to stabilize it. Over many years, it will deposit calcium (bone spurs) in or on the joint. This is because calcium is hard, and likely to prevent the excess motion the body is perceiving. Calcium deposits in or on a joint is the definition of osteoarthritis (calcium deposits in or on a joint), also known as degenerative arthritis.
Osteoarthritis (OA) is often diagnosed from an X-ray, which identifies the bony deposits. Many people have these types of calcium deposits on their X-ray images, without necessarily noticing any pain or symptoms. However, for others, OA progresses and may result in restricted movement and pain. You see, the calcium spurring creates an irregular stress and wear pattern on the joint surface (especially load bearing joints such as knees and hips), which can eventually break down protective cartilage.
This uneven stress on the joint will then stimulate even more calcium spurring and OA because of Wolff’s law (named after Dr. Julius Wolff) which states “Bones respond to stress by making new bone.”[8] Therefore, the presence of OA in a joint, over time, has a tendency to worsen the degeneration and OA in that joint.
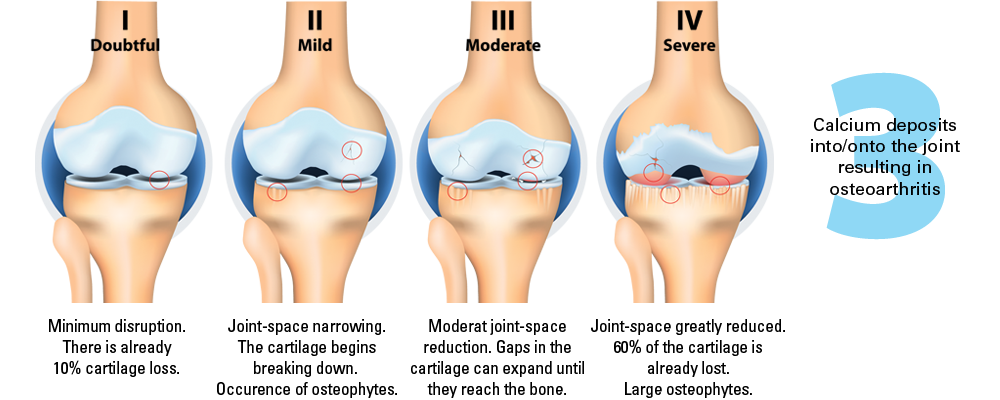
As you can see, osteoarthritis is not just a disease of cartilage breakdown, as many people believe, but rather one of connective tissue instability.[9] And there is a direct relationship between connective tissue injury, joint instability and the later development and progression of osteoarthritis .
The Importance of Joint Stability
How Prolotherapy Regenerative Medicine Helps
Prolotherapy stimulates the repair of injured or weakened connective tissue, which increases joint stability.[11] When ligaments and tendons are strong again, undesirable phenomena such as muscle spasm, fluid swelling, or aggravation of nearby nerves, triggered by the joint’s instability, often improves or resolves. Stress on other joints and body biomechanics also improves. Prolotherapy is also an excellent treatment for osteoarthritis (OA).[12] Prolotherapy treats the reason the arthritis developed (i.e., injured ligaments/tendons causing joint instability) as well as elevating growth-factor levels, helping the condition of cartilage. It is of course preferable to treat joint instability before OA develops.
However even if OA already exists, a remarkable thing has been observed after Prolotherapy: the pain often dramatically lessens or even goes away completely.[13]
In summary, the majority of chronic musculoskeletal pain comes from injured connective tissue that has not completely healed, resulting in joint instability, weakness, and eventually osteoarthritis. Prolotherapy “wakes up” these incompletely healed and painful joint connective tissue areas, restarting repair even years after the initial injury—reducing or eliminating pain.
Bibliography
[[1] Andriacchi T, Sabiston P, DeHaven K, Dahners L, Woo S, Frank C, Oakes B, Brand R, Lewis J. Ligament: Injury and repair. In Injury and Repair of the Musculoskeletal Soft Tissues (pp. 103–128). Park Ridge, Illinois: American Academy of Orthopedic Surgeons, 1988.
[2] Taber’s Cyclopedic Medical Dictionary, 18th ed. s.v. Definition of Collagen (p. 411). Philadelphia, Pennsylvania: F.A. Davis Company, 1997..
[3] Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. Journal of Pain. 2013 Dec 31; 14(12): 1539–1552.
[4] Jorgensen LN, Kallehave F, Christensen E, Siana JE, Gottrup F. Less collagen production in smokers. Surgery. 1998 Apr 30; 123(4): 450–455.
[5] Silverstein P. Smoking and wound healing. American Journal of Medicine. 1992 Jul 15; 93(1): S22–S24.
[6] Jam, B. Questioning the use of NSAIDs given inflammation is a perfectly healthy response following acute musculoskeletal injuries. 2014 Jul 14 [cited 2022 Mar 19] researchgate.net Banks AR. A rationale for prolotherapy. Journal of Orthopaedic Medicine. 1991; 13(3): 55–59.
[7] Stovitz SD, Johnson RJ. NSAIDs and musculoskeletal treatment: What is the clinical evidence? The Physician and Sportsmedicine. 2003; 31(1): 35–52.
[8] Cervoni TD, Martire JR, Curl LA, McFarland EG. Recognizing upper-extremity stress lesions. Physician and Sportsmedicine. 1997 Aug 1; 25(8): 69–86.
[9] Blalock D, Miller A, Tilley M, Wang J. Joint instability and osteoarthritis. Clinical Medical Insights Arthritis Musculoskeletal Disorder. 2015 Feb 19; 8: 15–23; Farrow CD, Newton CD. Ligamentous injury (sprain). In Textbook of Small Animal Orthopaedics. Ithaca, New York: International Veterinary Information Service, 1985.
[10] Hauser RA, Blakemore PJ, Wang J, Steilen D. Structural basis of joint instability as cause for chronic musculoskeletal pain and its successful treatment with regenerative injection therapy (prolotherapy). Open Pain Journal. 2014; 7:9–22 [cited 2022 Mar 19] benthamopen.com
[11] Soliman DMI, Sherif NM, Omar OH, El Zohiery AK. Healing effects of prolotherapy in treatment of knee osteoarthritis healing effects of prolotherapy in treatment of knee osteoarthritis. Egyptian Rheumatology Rehabilitation. 2016; 43(2): 47.
[12] Linetsky FS, Botwin K, Gorfine L, Jay GW, McComb B, Miguel R, Mikulinksky A, Parris W, Pollak S, Ray A, Saberski L, Taraschi P, Torres F, Trescot A. Position paper: Regenerative injection therapy (RIT) effectiveness and appropriate usage. Pain Clinic Magazine. 2002 June; 4(3): 38–45; Reeves KD, Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Alternative Therapies. 2000; 6(2): 68–79; Reeves KD, Hassanein K. Randomized prospective placebo controlled double blind study of dextrose prolotherapy for osteoarthritic thumbs and finger (DIP, PIP and Trapeziometacarpal) joints: Evidence of clinical efficacy. Journal of Alternative and Complementary Medicine. 2000; 6(4): 311–320.
[13] Hassan F, Trebinjac S, Murrell WD, Maffulli N. The effectiveness of prolotherapy in treating knee osteoarthritis in adults: a systematic review. British Medical Bulletin. 2017 Mar 4; 122(1): 91–108.