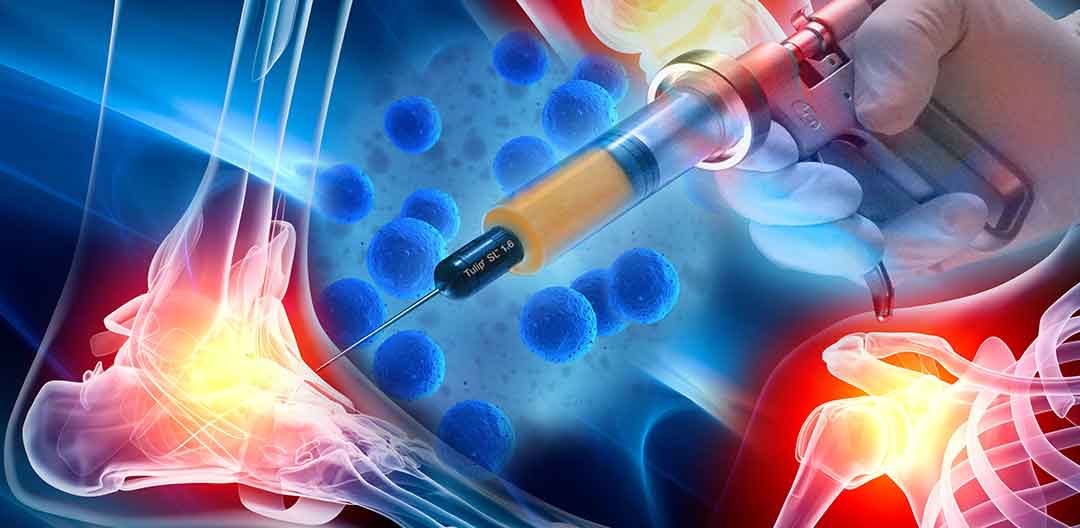
Biocellular Safety Concerns/Risk
As with any medical procedure, Biocellular Prolotherapy involves some risk, although when done by a properly trained professional, the risk is low. There is the risk of bruising and mild discomfort at the extraction site; this typically lasts for a few days up to perhaps a few weeks, but rarely longer. There is also the risk of infection at the extraction site, but this is extremely rare. An additional risk when extracting adipose could be minimal skin surface irregularity or dimpling at the fat extraction site, but since the amount of fat needed is so small, this is also extremely rare, especially when done by an experienced physician. With bone marrow extraction, there is the risk that the extraction site may remain sore for a period of time, however this is not common.
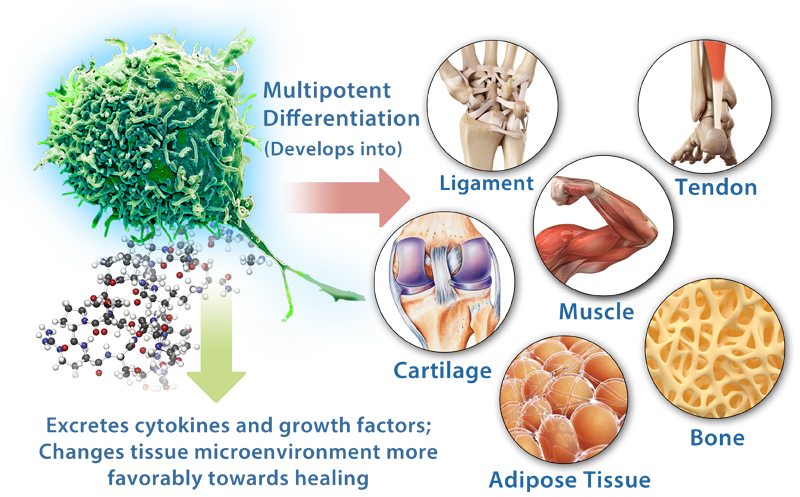
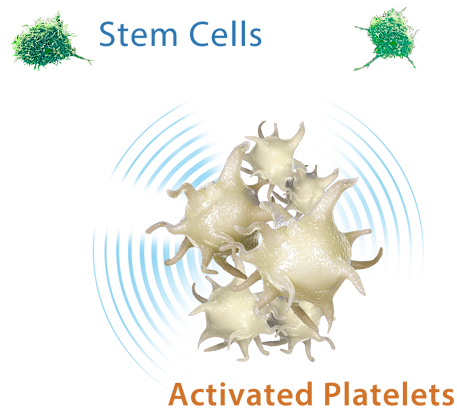
The question of safety also arises whenever cells capable of growth are introduced into a person. However, taking a person’s own stem cell-rich tissues and then giving them back to that same person has been shown to be very safe. One study monitored 1,873 patients for 21 years who had been treated with bone marrow cells between 1990 to 2006. During that monitoring period, the researchers found “no increased cancer risk” either at the treatment site or elsewhere.[41] Another study followed 91 patients for over two years who had been treated for various orthopedic conditions with adipose-derived cells mixed with platelet-rich plasma and found no tumor formation at any site treated (a total of 100 joints).[42]
Both bone marrow and adipose stem cells have also been used to repair injured cardiac muscle. As of 2014, more than 700 heart disease patients worldwide have received adult stem cell–based therapies with no indication of tumor growth ever reported.[43] In 2016, the Journal of Orthopaedic Surgery and Research concluded that the “use of MSC’s in the clinical setting can be considered safe, since no major adverse events related to the treatment nor to the cell harvest have been reported”, and that regardless of cell source or method, studies showed a high success.[44]
A few other procedure-related risks involving the extraction and injection of cells during this type of procedure exist in theory. This includes the theoretical risk for a blood clot; however, at the time of this writing there have been zero such events reported with the use of the microcannula harvesting system (a gentle method used in extracting adipose). Nonetheless, all potential risks should be discussed prior to treatment with the physician performing the procedure.
.jpg)